A recent review of Medicaid Managed Care Organizations (MCOs) has revealed concerning trends in approving prior authorization requests for services. In 2019, MCOs denied one out of every eight requests for prior authorization of services, according to a report by the Office of the Inspector General (OIG).
Among the 115 MCOs examined in the review, 12 exhibited denial rates for prior authorization requests that exceeded 25% — twice the overall rate. This discrepancy in approval rates highlights potential disparities in access to essential health care services for Medicaid enrollees.
Despite the high number of denials, many state Medicaid agencies reported that they did not routinely review the appropriateness of MCO denials. Additionally, many still needed to have mechanisms in place to collect and monitor data on these decisions. More robust oversight is required, potentially allowing inappropriate denials to go undetected within the Medicaid-managed care system.
The OIG has recommended measures to improve enrollee protections and state oversight of prior authorization denials in Medicaid-managed care in response to these findings. These include:
States must regularly review the appropriateness of a sample of MCO prior authorization denials.
Mandating States to collect data on MCO prior authorization decisions.
Issuing guidance to states on utilizing MCO prior authorization data for oversight.
States must implement automatic external medical reviews of upheld MCO prior authorization denials.
In their official response, the Centers for Medicare & Medicaid Services (CMS) did not indicate concurrence with the first four recommendations. However, they agreed with the recommendation to collaborate with States to identify and address MCOs that may be issuing inappropriate prior authorization denials.
Senator Robert Casey (D-Pa.), who chairs the Senate Special Committee on Aging and U.S. Representative Frank Pallone Jr. (D-N.J.), Energy and Commerce Committee ranking member, has voiced concerns about the potential prioritization of MCOs’ financial interests over the needs of patients seeking care. “I’m deeply troubled by reports that Medicaid managed care plans denied an average of one out of every eight requests for treatment, more than double the rate of service denials in Medicare Advantage,” Pallone said in an earlier statement.
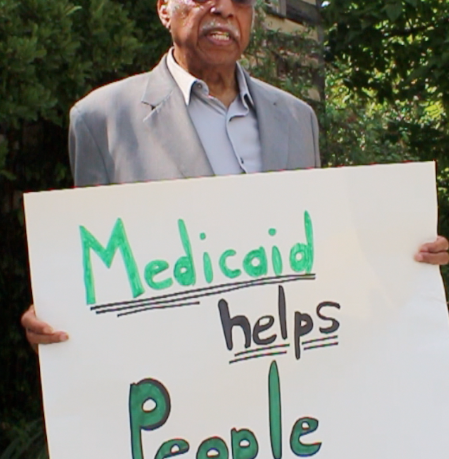
“Medicaid is a lifeline for over 80 million people, including children, people with disabilities, seniors, and hardworking families,” he continued. “This report strongly suggests that some private insurance plans, which states have contracted with to provide health care coverage to their residents, may be improperly denying access to critical services to maximize their profits.”
In a letter to the OIG, Casey emphasized the role of insurance companies in administering Medicaid benefits through MCOs, which receive fixed fees known as “capitated payments.”
Casey noted that independent watchdogs have consistently raised concerns about the MCO model, which may incentivize insurers to limit payments and deny coverage. He highlighted that MCOs have expanded significantly, becoming the “dominant delivery system” for Medicaid, providing coverage to over 67 million Americans, or 84% of Medicaid enrollees.
The senator noted that the OIG’s national evaluation of Medicaid MCOs, published in July, examined 115 plans with a minimum of 10,000 enrollees operating across 37 states and managed by seven companies. For example, the report found that, on average, MCOs denied 12.5 percent of requests for prior authorization in 2019, with notable variations from state to state and among different companies and plans.
Casey said one insurer in 13 states exhibited denial rates ranging from 5% to 29%. In California, denial rates for various MCOs ranged from 7% to 29%. The OIG report also identified 2.7 million individuals enrolled in MCOs with 25% or higher denial rates. Notably, one Illinois plan had a denial rate of 41%, while two other plans in Georgia and Texas denied one-third of claims.
Casey has called for a thorough examination of the MCO system to ensure that patients enrolled in Medicaid have unfettered access to the services they are entitled to. Additionally, he has urged the CMS to provide robust oversight to safeguard the interests of enrollees in receiving the care they need.
“When patients are denied coverage of medically necessary services, they often face tight timelines to file actionable appeals,” Casey said. “Assuming such appeals are filed in a timely manner, the process can be complicated and time-consuming, creating barriers that can make it difficult for Medicaid enrollees to seek recourse.”